Cities across the country are turning to innovative new approaches to address mental illness, substance use disorder, and homelessness, a new issue brief says, after more traditional responses — such as funneling vulnerable populations through jails and prisons — have proven less than effective.
The National League of Cities and Arnold Ventures released the first in a series of issue briefs examining city-level approaches to these interconnected challenges, which are immense in scope: More than 46 million U.S. adults lived with a mental illness in 2017, more than 20 million met the criteria for substance use disorder in 2014, and nearly 553,000 experienced homelessness on a single night in January 2018.
The human toll from substance use disorder has climbed to intolerable levels — deaths increased by more than 600 percent between 1980 and 2014. Meanwhile, the chronic conditions experienced due to homelessness can reduce an individual’s life expectancy by 17.5 years.
Mental illness, substance use disorder, and homelessness also pose a significant economic burden. Mental illness was associated with $200 billion in direct health care costs nationwide in 2013 — surpassing heart disease, cancer, and diabetes. Substance use accounts for $64 billion in annual health care costs and $340 billion in overall costs, such as crime and lost work productivity. The impact of a single person experiencing homelessness on public resources can reach between $30,000 and $50,000 per year.
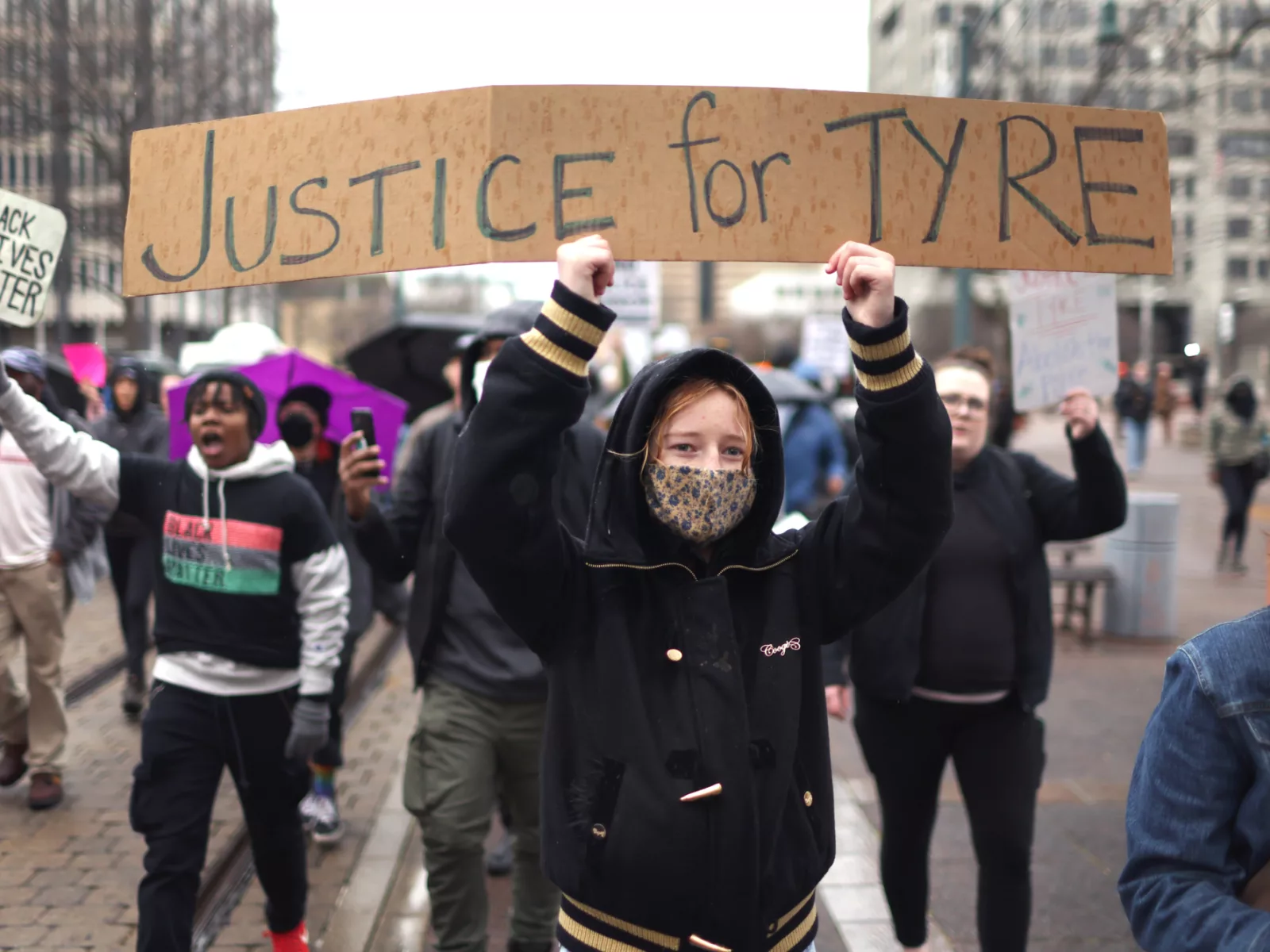
Even as homeless counts have trended downward over the past decade, the continuing opioid epidemic has placed strains on access to health care, housing, education, and other critical services. From Skid Row in Los Angeles to tent camps in Washington D.C., cities have been on the front lines of this all-too-visible and seemingly intractable policy problem. It is critical that local governments move away from punitive responses and embrace effective policies to better respond to vulnerable populations, the brief says.
Cities have begun to craft some unique strategies specifically tailored to local needs:
- In First Responder-Provider Partnerships, police and other first responders collaborate with mental health providers when serving individuals with mental illness, substance use disorder, or those experiencing homelessness. These partnerships can take different forms. For example, officers in Seattle’s Crisis Response Unit receive special Crisis Intervention Team training and work closely with mental health experts to triage cases. In Boston’s co-responder initiative, master’s‑level clinicians ride along when police officers respond to calls involving mental illness.

- Some cities have implemented First Responder-Led Referral Programs, which allow people who want treatment for substance use disorders to seek help though police or fire departments without facing the threat of criminal liability for substance use. Under the Angel Program in Gloucester, Mass., police officers are trained to assist individuals who meet proper criteria connect to treatment programs.
- The struggle to properly address mental health has spurred cities to create Regional Dedicated Emergency Psychiatric Facilities, which serve as standalone departments that can serve psychiatric patients from different medical emergency facilities. In Alameda County, Calif., emergency responders can transport individuals undergoing a psychiatric emergency directly to the John George Psychiatric Hospital instead of a general hospital, reducing waiting times and improving outcomes.
The full brief is available here. Upcoming briefs will delve into specific approaches and begin to explore best practices.