Working at the intersection of health care, public health, and criminal justice, Arnold Ventures is collaborating with communities across the country to use data to develop treatment programs for individuals with complex needs.
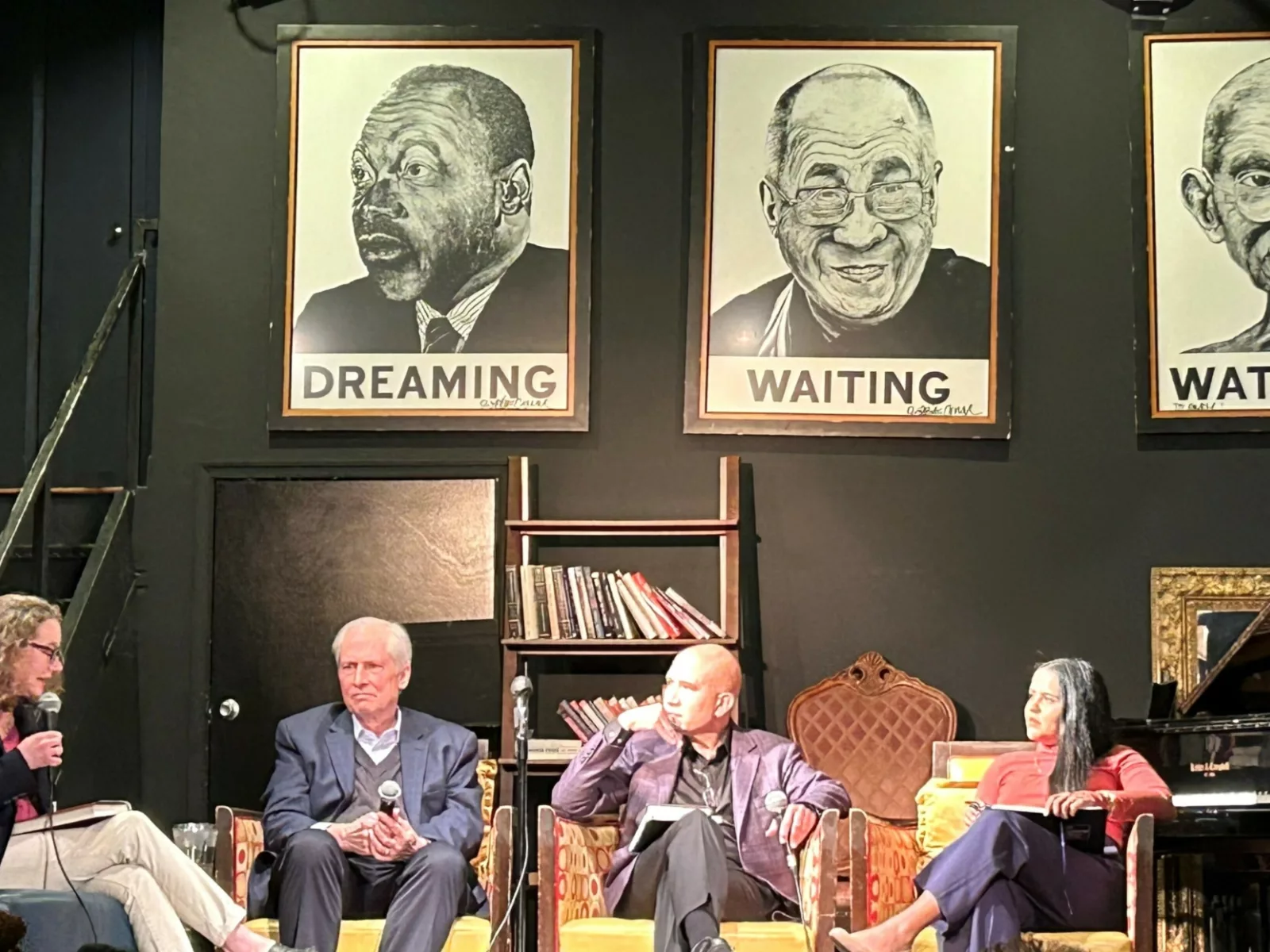
Health Care Director Erica Socker, Public Health Managers Julie Williams and Sarah Twardock, and Criminal Justice Manager Catie Bialick spoke recently at Johns Hopkins University about the gap between evidence and practice across numerous areas, including homelessness, the opioid epidemic, and the emergency response system.
Below are three highlights from the panel discussion.
1. Evidence says this approach saves lives — but only 40 jails offer it
“There’s a study … that looked at thousands of people [with opioid use disorder] who got methadone and buprenorphine post-release [from jail]. They found that people who didn’t get that medication were 129 times more likely to fatally overdose the first two weeks post-release.”
— Julie Williams, Public Health Manager
Despite the fact that giving medication to people with opioid use disorder who are incarcerated could save lives, Williams said, fewer than 40 jails in the U.S. offer treatment programs.
“With that information, you can’t not take action,” Williams said.
Arnold Ventures has committed roughly $10 million to study how to improve the country’s treatment system for opioid use disorder. Now the philanthropy is exploring new ways to help the thousands of people who are jailed for drug use: It plans to support research on treatment programs in the corrections system and ways to expand community addiction services to help people after they are released.
2. Meet Joe: One man, 60 police interactions
“We have many stories of individuals — like a gentleman named Joe, from Cambridge, Massachusetts, who over the course of two years, had 60 different case notes from police interactions that led to only one arrest. This is just one example of how police are doing a lot to try to … help these individuals, but they might not have the resources they need.”
— Catie Bialick, Criminal Justice Manager
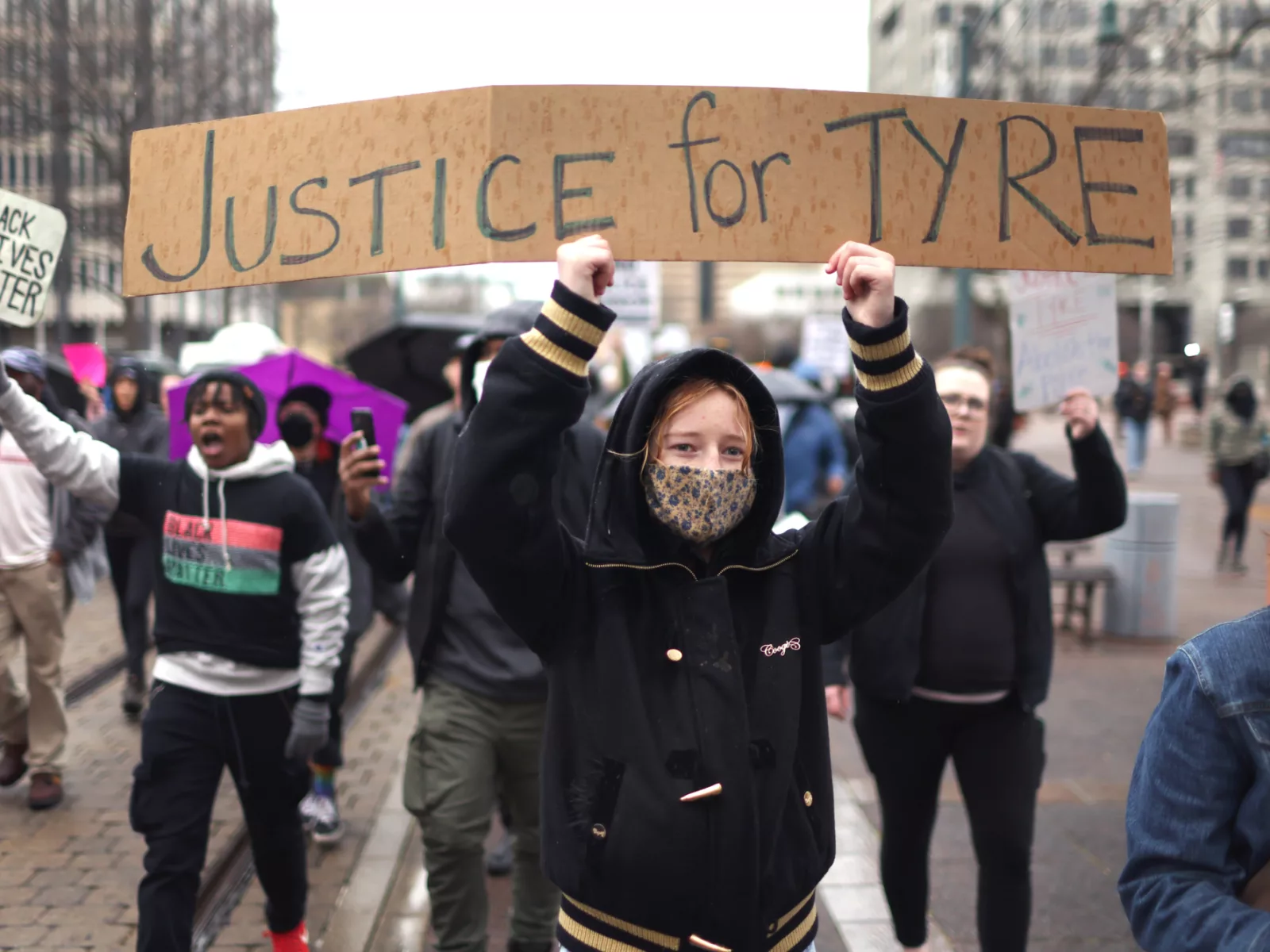
Police and other first responders across the country are stepping in to help individuals with serious behavioral, mental, or physical health problems who have nowhere to turn for help but to emergency systems.
The challenge many of these departments face is there are limited long-term care options for these people except jails or emergency rooms, Bialick said. And there is no network of services that first responders could rely on as an alternative to arresting or hospitalizing a person.
The philanthropy is working with local and regional officials in several communities across the country to use data to better understand the needs of “frequent utilizers,” improve coordination among local crisis response teams and social service providers, and develop research-based treatment programs to help people lead more stable lives.
3. Complex populations require coordinated policies, integrated services
“This [the complex care population] is the 5 percent of patients that drive 50 percent of health care spending. You can think of a lot of different ways to approach this population as a funder and to … segment it. We’re focusing on the dual eligibles in the near term; the group of patients who are simultaneously eligible for both Medicare and Medicaid.”
— Erica Socker, Director of Health Care
Within the health care system, there is a small subset of individuals with complex medical, behavioral, and social needs that accounts for a disproportionate share of spending, Socker said. This group includes people with disabilities and multiple chronic conditions.
Socker and her colleagues are working with officials to develop federal and state policies intended to improve coordination and patient outcomes across acute care, long-term support services, home care, and behavioral health services. Their main goal is to spend money more effectively to achieve better patient outcomes at the same or lower cost.
The team is looking to better integrate the array of services these patients receive through changes to payment and delivery systems. They are working to find ways to link medical and social services, such as housing, nutrition, and transportation, in an effort to remove barriers that prevent people from getting treatment and managing their own health.
Twardock also spoke about changing Medicaid policy at the state level to increase access to care for those with opioid use disorder.